Abstract
Background: Primary immune thrombocytopenia (ITP) is an immune-mediated acquired disorder characterized by impaired production and increased destruction of platelets with an elevated risk of bleeding. At present, diagnosis of primary ITP still remains one of exclusion with a need to discard other causes of isolated thrombocytopenia, in the absence of robust and accurate clinical and laboratory diagnostic criteria. For the diagnosis of ITP, a bone marrow (BM) study may be useful to differentiate between ITP and other diseases, such as myelodysplastic syndromes (MDS). Next generation flow (NGF) has emerged as a potential useful tool in these settings.
Aim: In this study (FCR-PTI-2017-01) we prospectively evaluated the potential utility of NGF analysis of BM and peripheral blood (PB) for more accurate diagnosis of ITP vs MDS.
Methods: 62 patients presenting with isolated thrombocytopenia and classified as ITP (n=20), MDS (n= 11) or inconclusive, i.e. unclassifiable, (n= 25) by BM cytomorphology, were studied. PB (n=47) and BM (n=62) analysis by NGF was blindly performed in parallel for the ITP, MDS and unclassifiable patient groups using the EuroFlow 8-colour AML/MDS classification antibody panel followed by automated analysis against pre-existing flow cytometry databases of normal healthy donor PB and BM immunophenotypic profiles. NGF BM and PB results were then compared with the BM cytomorphological diagnosis. In parallel, epidemiological data from patients were recorded in an electronic case report form (eCRF) and analyzed afterwards.
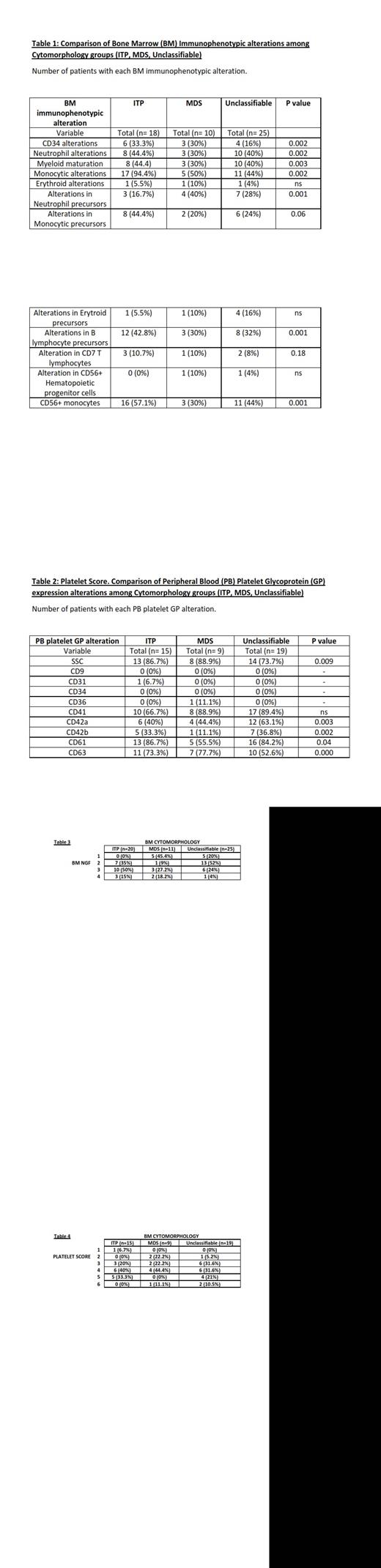
Results: By cytomorphology, expert hematologists were able to conclude an ITP or MDS diagnosis in only 31 cases (55.3%). 62 BM and 48 PB samples with isolated thrombocytopenia were evaluated by NGF. Our 62 patients were allocated in 4 immunophenotypic groups attending to different BM variables observed: maturation blockades, abnormal antigen expression and cross lineage markers. Thus, we observed normal phenotype cases (n=10), isolated (unilineage) alterations (n=24), mild multilineage (>1) alterations (n=20) and severe multilineage (MDS-like) phenotypes (n=8). Cytomorphology diagnosed our cases as ITP, MDS or unclassifiable with a median number of alterations observed by BM NGF of 4 (IQR, 3-6), 2 (IQR, 1-6) and 4 (IQR, 3-5) respectively. For ITP cytomorphology group, NGF demonstrated numerous BM alterations being monocytic alterations (n=17, 94%) the most frequent finding observed. MDS presumed cases were also associated with monocytic alterations (50%) with a frequent decrease in neutrophil precursors (40%). On the contrary, when cytomorphology was not capable to establish a diagnosis, NGF showed a mixture of alterations with no clear predominance of none of them (table 1). Similarly to our work with BM NGF, we looked into a potential correlation of cytomorphology with PB NGF phenotypes. Thus, we observed a median number of alterations of 4 (IQR, 3-5), 4 (IQR, 2-4) and 4 (IQR, 3-5) in ITP, MDS and inconclusive cytomorphology groups. Increased platelet size and upregulated CD41, CD61 and CD63 glycoprotein (GP) expression were the most characteristic findings of ITP cohort. MDS subtype depicted an increased platelet size and overexpression of CD41. Downregulation of GP was restricted to patients with MDS-like phenotypes. (table 2). Nearly statistical significant differences at significance level of 90% were observed between cytomorphology and BM NGF results (p=0.179) (table 3), between platelet score and BM NGF findings (p=0.118) and also, among morphology, BM NGF and platelet score (p=0.179). Nevertheless, cytomorphology and PB NGF showed no statistical differences between them (p=0.206) (table 4).
Conclusions: Limitations of BM cytomorphology when facing an isolated thrombocytopenia were demonstrated here. However, normal or unilineage BM NGF alterations may lead us to an ITP diagnosis while mild or severe multilineage BM phenotypes may correlate good with MDS. PB platelet GP expression allowed us to classify our patients in six groups (Gonzalez-Lopez/Matarraz platelet score) which may help ITP diagnosis when this score is low. Comparison of BM cytomorphology, BM NGF and PB NGF techniques at diagnosis showed statistically nearly comparable results (p=0.179), with a bigger amount of patients needed to confirm this trend. All these NGF findings may lead us to better address ITP at diagnosis.
Gonzalez-Lopez: Novartis: Other: Advisoryboard and speakers honoraria, Research Funding; Amgen: Other: Advisory board and speakers honoraria, Research Funding; Sobi: Other: Advisory board honoraria; Grifols: Other: Advisory board honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal